Breadcrumb
Foreign Materials in Gingival Lesions
What is it?
Research on certain persistent gingival (gum) lesions.
What problem does it aim to solve?
Some patients have lesions on their gums that don’t improve after periodontal treatment and careful oral hygiene practices. This research aimed to understand why these lesions were appearing and not healing. Because foreign particles were being frequently observed, the researchers focused on this aspect.
How does it work?
Biopsy specimens containing foreign particles submitted to the Dugoni School’s pathology lab were selected and subjected to a battery of imaging and assaying techniques. They were also compared to a set of control specimens in which no particles had been detected. The findings were that most of the lesions were white, and described as plaques. There also tended to be multiple lesions and chronic inflammation present. When the foreign particles in the specimens were analyzed, silica turned out to be the predominant element. Lesions in the study samples were far more likely to have been diagnosed as leukoplakia, or pre-malignant, than those in the control group. The researchers also looked at the in vitro effects of silica on gingival fibroblast cells and found that exposure caused the cells to release higher amounts of inflammatory cytokines.
What are the real-world implications?
Silica is already known to cause harmful effects in the human body; it seems to be causing inflammatory effects — and lesions — in people’s mouths as well. Silica is prevalent in dental materials and over-the-counter oral hygiene products, which is likely how these particles are ending up in mouths.
What are the next steps?
More research needs to be done. In the meantime, oral health professionals should be mindful of the risks from these particles in their practice and when recommending oral healthcare products and treatments.
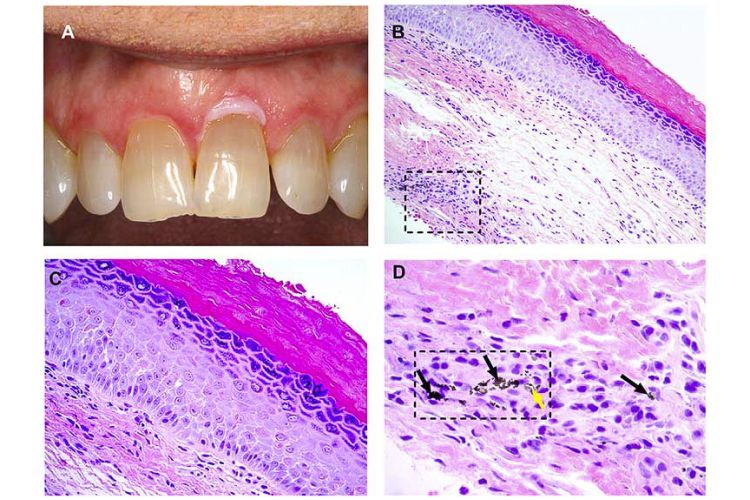
Fig. 1. (A) Clinical image showing a white lesion involving the facial marginal gingiva of tooth #9. (Courtesy of Dr. Reid Lester). (B) Representative photomicrograph showing hyperorthokeratosis and foreign material in the deep lamina propria (square) (hematoxylin and eosin [H&E]; original magnification £ 200). (C) High-power view of the same case shows that the epithelium exhibits dyskeratosis, cellular discohesion, and nuclear pleomorphism limited to the lower one-third of the epithelial thickness—mild dysplasia (H&E; original magnification £ 400). (D) High-power view of the square area of image B, reveals that the foreign material consists of very fine, blackish granules (black arrows) accompanied by slightly larger, colorless, refractile, crystalloid particles (yellow arrow) (H&E; original magnification £ 800). A high-resolution version of the image is available as eSlide: VM05618.
Source
“Investigation of foreign materials in gingival lesions: a clinicopathologic, energy-dispersive microanalysis of the lesions and in vitro confirmation of pro-inflammatory effects of the foreign materials”, Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, Volume 128, Issue 3, September 2019, Pages 250-267
Authors
Leticia Ferreira, DDS, MS, Department of Diagnostic Sciences, University of Pacific Arthur A. Dugoni School of Dentistry
Hsin-Hsin Peng, PhD, Center for Molecular and Clinical Immunology, Chang Gung University, Taiwan; Laboratory Animal Center, Chang Gung Memorial Hospital, Taiwan
Darren P. Cox, DDS, MBA, Department of Diagnostic Sciences, University of Pacific Arthur A. Dugoni School of Dentistry
David W. Chambers, EdM, MBA, PhD, Department of Orthodontics, University of Pacific Arthur A. Dugoni School of Dentistry
Avni Bhula, DDS, International Dental Studies Program, University of Pacific Arthur A. Dugoni School of Dentistry; Department of Oral and Maxillofacial Radiology, University of California, Los Angeles
John D. Young, MD, PhD, Center for Molecular and Clinical Immunology, Chang Gung University, Taiwan; Laboratory of Cellular Physiology and Immunology, The Rockefeller University, New York
David M. Ojcius, PhD, Department of Biomedical Sciences, University of Pacific Arthur A. Dugoni School of Dentistry
Erivan S. Ramos-Junior, DDS, MS, PhD, Department of Biomedical Sciences, University of Pacific Arthur A. Dugoni School of Dentistry
Ana Carolina Morandini, DDS, MS, PhD, Department of Biomedical Sciences, University of Pacific Arthur A. Dugoni School of Dentistry

![Fig. 1. (A) Clinical image showing a white lesion involving the facial marginal gingiva of tooth #9. (Courtesy of Dr. Reid Lester). (B) Representative photomicrograph showing hyperorthokeratosis and foreign material in the deep lamina propria (square) (hematoxylin and eosin [H&E]; original magnification £ 200). (C) High-power view of the same case shows that the epithelium exhibits dyskeratosis, cellular discohesion, and nuclear pleomorphism limited to the lower one-third of the epithelial thickness—mild dy](/sites/default/files/styles/mobile_header_image/public/2020-09/particles-research-main.jpg?itok=QE4kfgJ4)



