The Pacific Center for Equity in Oral Health Care focuses on addressing the needs of those who remain vulnerable to poor oral health and the subsequent consequences to health and wellbeing due to limited access to oral health care. From its founding in 1990, the Pacific Center has prioritized and launched programs to address disparities in oral health care, diversification of the dental workforce and policies that support access to care. We contribute to the Dugoni School of Dentistry’s legacy of humanism and commitment to courage, excellence, empowerment, integrity, innovation and leadership.
The goal is to remove barriers to oral health care for those who need it most. Dugoni faculty, students, staff and alumni collaborate with other leaders in education, healthcare, policy and research. This work has resulted in the development of alternative care delivery models; sustained advocacy for the integration of oral care with primary care; expanded use of teledentistry; development of pathway programs in dental education toward a more diverse, inclusive and effective workforce; creation of timely curricula and support for policies that improve resources and access to oral health care for all. The Pacific Center will continue this work to contribute to and influence local, state, national and international efforts toward increased and more equitable access to those resources as an integral part of healthcare.

A Guide for Clinicians
The National Roadmap for Disability-Inclusive Healthcare is a plan created for clinicians to give the best healthcare possible to people with intellectual and/or developmental disabilities (IDD).

Geriatric Dental Medicine for Baby Boomers
Article by Dr. Elisa M. Chavez, "Oral health issues of late Baby Boomers (1956–1964)" in Special Care in Dentistry's special issue Geriatric Dental Medicine for Baby Boomers.

Racism and Bias in Dentistry: A Call to Action
This document is a summation of action items and strategies generated by participants in the Racism and Bias in Dentistry Symposium at the Dugoni School. The dentistry community can use this as a means to address biases in dental practices and beyond.
Read more
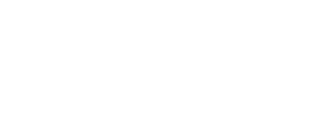
Our dental programs are an important component of the safety net in the communities we serve. Many of our patients travel from underserved areas to access care from our outstanding faculty and students.
Tens of thousands of patients across Northern California seek dental care in the Dugoni School's dental clinics and many more are served through collaborations with local partners dedicated to serving those who face challenges accessing affordable oral health care, such as La Clinica De La Raza, On Lok PACE and San Mateo Medical Center. Our dental programs are an important component of the safety net in the communities we serve not only because of our reduced fees, but because of our faculty who are experts in caring for those with special or complex medical and dental needs.
Many who seek care in our clinics or from our partners have been unable to establish a dental home in the past. Some because of limited financial resources, some because of complex medical or social issues and some because there is not a provider closer to their home or one who can manage their needs. Our students and faculty care for patients with special and complex needs in our Special Care and Hospital Dentistry and Union City clinics. The Pacific Center has also developed resources for caregivers, such as Overcoming Obstacles training materials, created to help establish appropriate and effective daily oral care plans and homecare strategies for those who are most vulnerable to oral diseases.
The Pacific Center’s pathway programs will enhance the diversity of our dental workforce and create educational programs that help our students and alumni reach vulnerable populations and those with health and psychosocial considerations that make accessing or receiving dental care a challenge. The Dugoni School has long provided didactic and clinical experiences for students and practitioners to improve their ability to care for individuals at every level of ability and every stage of life. From continuous improvement in curriculum design and delivery, to clinical experiences through our on-campus Special Care and Hospital Dentistry clinic and working with community partners caring for underserved communities, children and frail older adults off-site, Dugoni graduates learn to prioritize and care for diverse populations — and they are uniquely poised to contribute and lead in their communities.

We provide a comprehensive curriculum focusing on the care of medically compromised individuals and other populations with limited access to dental services, from pediatrics to geriatrics.
Dugoni School graduates are prepared to serve patients with complex needs in any setting, as part of an interprofessional team. Extramural and inter-professional rotations prepare our graduates to work in hospital settings, long term care, community health clinics and mobile dentistry.
Telehealth programs prepare all practitioners to extend their reach beyond the walls of their practices to those most in need. In addition to our pre- and post-doctoral programs, dental hygiene and our International Dental Studies programs, the dental school provides a wide array of advanced education and continuing education courses for every member of the dental team to improve their knowledge and skills in working with vulnerable populations.
Our Advanced Education in General Dentistry program prepares its graduates to manage patients with complex dental and medical issues in diverse settings. Our Registered Dental Hygienist in Alternative Practice program was developed at the Dugoni School of Dentistry and prepares hygienists for more independent practice in community settings as part of a team focused on improving access to care for those most challenged to travel from their homes or communities for oral health care.

Policies Supporting Oral Health in Aging Populations Are Needed Worldwide
A new study coauthored by Dr. Elisa Chavez in the International Dental Journal.

Dugoni among first dental schools to train students on treating people with disabilities
The Dugoni School is a pioneer in teaching how to treat patients with conditions making it difficult for them to access care.
Why a Dental Benefit Is Still Needed for All
The need for and benefit of regular oral health care for older adults has been demonstrated time and again, but there remains a known gap in our health care system that continues present barriers.

Oral Health in America
The report details the unequal burden of oral health conditions across population groups and highlights promising new directions for health care delivery.
Interdisciplinary Oral Healthcare
Dr Allen Wong and Dr Lisa Itaya have co-authored an article, "Interdisciplinary Oral Health for Those with Special Health Care Needs" in the North American Dental Journal
Delivering on the Promise of Teledentistry
The Dugoni School’s work in telehealth is featured prominently in a new ADEA policy report.

Stanislaus and Merced Counties Face Dental Provider Shortages
Legacy Health Endowment (LHE) and the EMC Health Foundation collaborated with the University of the Pacific School of Dentistry to create a report that examines the current and future dental needs of children and the elderly across Stanislaus and Merced Counties and how best to bring more accessible and affordable dental care services to people in need.

Older Adults
The Pacific Center and California Dental Association convened a gathering of experts and stakeholders in October 2019 to conduct an analysis of oral health needs, dental education, workforce, financial and reimbursement structures and legislative opportunities as they relate to older adults in California. Proceedings authored by Dr. Chávez, Dr. Michelle Brady and Dr. Paul Subar are now published in the Journal of the California Dental Association.
Health Policy
The Pacific Center advocates for new and reformed health policy toward the inclusion of oral health care as an integral and meaningful part of the healthcare system, available to all. Through collaborative work with community partners and engagement with local, state, national and international leaders, the Pacific Center engages in projects to address unmet needs among some populations and disparities in oral health care resources within the healthcare system. Over time, some of these collaborations and the participation of Dugoni School faculty and staff have produced results such as the classification of RDHAP as a new level of provider in California, wider acceptance and use of telehealth, expanded access to care through the Medi-Cal Dental Program and most recently an acknowledgement of medically necessary dental care as the 2023 Medicare Physician Fee Schedule will for the first time include coverage for dental services (which have been explicitly excluded since its inception) that are related to organ transplant surgery, cardiac valve replacement, valvuloplasty procedures and head and neck cancers.

CDA Journal Focuses on DEIB
Dr. Elisa Chávez has an article in the October issue of the Journal of the California Dental Association: "Improving Access to Care and Patient Experience Through Diversity, Equity, Inclusion and Belonging"

Patients with IDD
"Although the American Dental Association (ADA) guarantees equal access to oral healthcare for all individuals, unfortunately, the reality is that access is disproportionately reduced for many Americans with intellectual and developmental disabilities (IDDs)..."
NCD announces policymaker blueprint for health equity for people with disabilities
The National Council on Disability has released a framework for policymakers, calling for an all-of-government approach to longstanding medical discrimination against people with disabilities.

Racism and Health
Racism is the reason for large, sustained health inequities in the US. Four overview articles in this month’s Health Affairs orient the reader to the complex relationship between racism and health.

Affording Dental Care
Recent studies from the ADA Health Policy Institute show that while children are reported to have fewer financial barriers to oral health care, barriers for adults have increased since 2005.
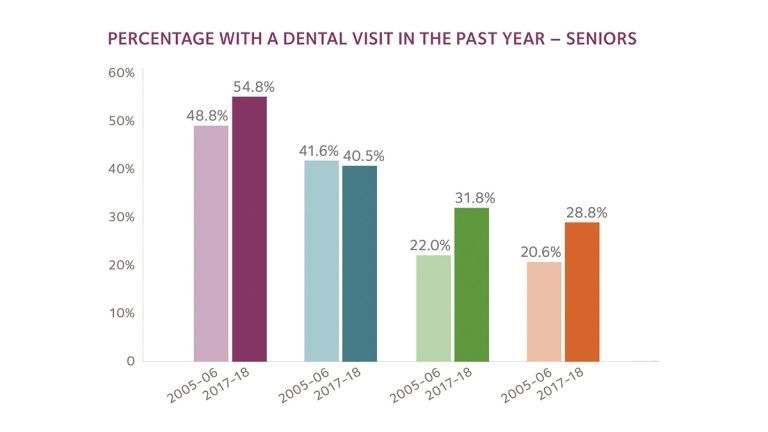
Accessing Dental Care
Money-related obstacles to oral health care are highest among older adults. Racial disparities in dental utilization are most pronounced for Hispanic older adults.

Underrepresentation
Hispanic and Black dentists remain significantly underrepresented among the general population. Enrollment of Hispanic and Asian students has increased since 2005 across all U.S. dental schools, but enrollment of Black students remains at 6.2%, even though 12.4% of the U.S. population is Black.

Student Debt
Educational debt levels for dental student graduates vary significantly by race. More than 20% of Asian dentists graduate with no student debt compared to less than 1% of Black dentists. Black dentists, by far, graduate with the highest levels of educational debt.
Contact Us

155 Fifth St.
San Francisco, CA 94103